Solid Lipid Nanoparticles
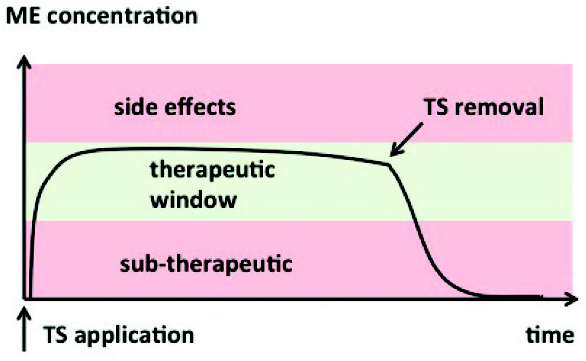
Solid lipid nanoparticles (SLN) are a type of a carrier system that employs solid lipids as a matrix for drug delivery.1 The drug is molecularly dispersed within the lipid matrix, and the system is stabilized with an emulsifier.2 Nanoparticles distributed within the matrix usually have a mean particle size between 50 and 1000 nanometers.3,4 This reduction in particle size along with drug incorporation throughout the lipid matrix provides relevant pharmaceutical features to SLN as a drug delivery system. While decreased particle size leads to an increase in surface area attributing to an improved drug release profile, the degree of drug dispersion within the lipid matrix can be manipulated to control the drug release rate.5 SLN combine the benefits of their counterpart nanoparticle carrier systems while minimizing potential formulation problems. The advantages of SLN include improved drug-carrier stability, protection of incorporated drug from degradation along with enhanced tolerability, controlled drug delivery, and site-specific targeting.6 The pharmaceutical market is potentially expanded for this drug delivery system because the production of SLN allows for the incorporation of both lipophilic and hydrophilic drugs. Formulation using physiologic lipids eliminates the need for organic solvents, thus mitigating the potential for carrier toxicity. The ease of large-scale manufacturing along with feasibility of drug delivery through various routes of administration complements the progression of this drug delivery system.5,7
Role of Lipids in the Development of Solid Lipid Nanoparticles
Poorly water soluble drugs have limited dissolution and bioavailability. In contrast to polymeric drug carriers, lipids are more physiological and biocompatible carriers that may aid in the resolution of this issue. Moreover, the reduction in size of SLN can be attributed to enhanced particle adhesion to the gut wall, a location more suitable for drug release and absorption. Apart from promoting absorption, lipids are degraded by gut enzymes creating micelles. Solubility enhancement occurs as the lipid matrix (containing the dissolved drug) is incorporated into these micelles. Upon lipid degradation, the drug is released and absorbed.3 Figure 1 shows the effect of lipids on drug absorption. The solid lipids used to prepare SLN are crystalline in nature and serve as the matrix in which an immobilized drug is molecularly dispersed. Stability of SLN is influenced by the bulk properties and the length of their composite lipids. Short lipid chains with less branching degrade more quickly in comparison to long lipid chains with more branching.8 Further, the inclusion of lipids helps to improve not only drug solubility, but also drug loading and drug entrapment efficiency of SLN.9 Considerations such as lipophilicity, viscosity, contact angle, and chain length of the incorporated lipid must be examined prior to preparation. The lipid should have some degree of lipophilic character in order to solubilize a lipophilic drug and incorporate the drug into the SLN. Highly viscous lipids may be problematic during the formulation process, requiring procedures that may lead to drug degradation. Lipids with a high contact angle may adversely affect the stability and production of nanoparticles.9 In a study by Prasad et al,10 lipid chain length was found to influence drug supersaturation levels and precipitation inhibition in self-emulsifying drug delivery systems. Thus, the appropriate selection of lipids for the preparation of SLN is important for a successful formulation. Zoom In
Zoom In
Figure 1. The effects of lipids in prepared SLN on drug absorption.
Role of Polymers in the Development of Solid Lipid Nanoparticles
The use of polymers in the formulation of nanoparticles has fallen out of favor due to toxicity concerns, the high cost of biodegradable polymers, and difficulty with large-scale production.11 Despite these drawbacks, polymers have been used as surfactants to stabilize SLN. Poloxamer and polysorbate 80 are 2 examples of surfactants approved for use that are generally well tolerated.11 Surface coating with polymers, such as polyethylene glycol (PEG), is used to increase biodistribution by modifying hydrophobic particles located on the surface of SLN and stabilizing them. As an amphiphilic copolymer, PEG is capable of orienting its hydrophobic residues near the lipophilic SLN core. The strength of the bonds formed between SLN and the polymer determine the SLN stability, prevention of agglomeration, and dispersability. Surface modification also provides increased transport and site-specific drug targeting.12
Drug-Lipid Miscibility
Lipid-based formulations can be used to increase drug absorption by increasing solubilization, enhancing permeability, reducing drug metabolism by inhibiting hepatic enzymes, and improving transport via the inhibition of efflux transporters and an escalation of chylomicron production.13Figure 2 highlights the pharmaceutical and pharmacologic implications of evaluating drug-lipid miscibility in solid lipid nanoparticles. The miscibility of a drug and excipient is found to be dependent upon the intermolecular interactions formed between the drug (solute) and excipient (solvent).14 Miscibility can be an essential component for the formulation stability of SLN. Mixed glycerides, such as glyceryl monooleate (GMO), serve as a popular solvent for poorly water soluble drugs. GMO is a waxy, long-chain glyceride useful in formulating liquid dosage forms. Sorbitan fatty acids (Spans) have similar physical properties to GMO. These polar oils, also known as co-surfactants, promote miscibility due to the presence of hydroxyl groups.15Co-surfactants decrease interfacial tension between two immiscible components to improve thermodynamic stability and thus, miscibility.16 Shah and Agrawal identified excipient-drug compatibility as the most significant parameter affecting drug solubilization.14 Their study involving a hydrophilic drug, ciprofloxacin HCl, was assessed for compatibility with solid lipids, Dynasan 114, Dynasan 118, Monecol PC, Monosteol, Softemul 165, Geleol, and Imwitor 900. They reported that Geleol solubilized the drug the most due to the presence of oxygen and OH functional groups, which contributed to polar interactions and hydrogen bonding. The findings indicated a trend that increasing differences of total solubility parameters and polarity between the drug and lipid paralleled increased immiscibility.14 Zoom In
Zoom In
Figure 2. Pharmaceutical and pharmacologic implications of evaluating drug-lipid miscibility in solid lipid nanoparticles.
Drug-Polymer Miscibility
Drug-polymer miscibility, although not extensively considered by researchers during early stages of preformulation, plays an important role in the formulation of SLN. The miscibility of various drug-polymer complexes has usually been reported through the analysis of component interactions. To improve the physical stability of the drug, it must be mixed with a lipid matrix containing polymer to modify the environment surrounding the drug to provide more favorable conditions. In many cases during the lyophilization process, SLN are converted from the crystalline to the amorphous form. Polymers in these lyophilized SLN are capable of altering the chemical properties of the drug, which may lower the thermodynamic tendency for crystallization.17 In amorphous systems, polyvinylpyrrolidine (PVP) has been shown to form hydrogen bonds with nifedipine, a drug containing a N-H functional group. These interactions were shown to decrease molecular mobility and stabilize the drug carrier system. A similar principle can be applied to lyophilized SLN so as to stabilize them in amorphous form. However, it should be noted that preparation method, temperature, and drug-lipidpolymer composition can influence the miscibility between these components.18Extensive studies on this have been carried out by Marsac et al17 to examine various approaches to predict drug-polymer miscibility and solubility. Observations on the importance of molecular size were noted in relation to entropy of the system. The degree of enthalpic interactions or cohesive interactions determined the miscibility of the drug delivery system, including SLN more so than adhesive interactions formed from the drug-polymer mixture. The significance and strength of these interactions were dependent upon the chemistry of the drug and selected polymer. Immiscibility between components may warrant the use of an alternative polymer of lower molecular weight.17Moreover, drug-polymer molecular interactions affect the delivery system tendency to undergo precipitation or drug recrystallization.19 Studies conducted by Chauhan and colleagues correlated the effects of polymers in relation to precipitation and recrystallization inhibition using dipyridamole (DPD) in conjunction with the following polymers: PVP K90, HPMC, Eudragit E100, Eudragit S100, Eudragit L100, and PEG 8000. Eudragit E100, HPMC, and Eudragit S100 were found to significantly improve precipitation inhibition efficiency by increasing the time to initiation and decreasing the rate of precipitation. This was attributed to hydrogen bonds formed between DPD C–N or O–H functional groups and polymers.19 Similar studies assessing the contribution of polymeric drug interactions between indomethacin (IMC) and PVP K90, HPMC, Eudragit E100, Eudragit S100, Eudragit L100, and PEG 8000 were analyzed by Chauhan et al. It was determined that increased hydrophobicity of polymeric excipients correlated with a limited ability to form necessary interactions with IMC polar groups to inhibit nucleation.20 Further, these interactions were associated with enhanced solubility and stability in the presence of lower polymer concentrations as a result of limited steric hindrance and increased capacity to form molecular interactions.20
Other Excipients Used in the Preparation of Solid Lipid Nanoparticles
Arrays of excipients are available for the preparation of SLN. Selection of the most appropriate excipient is dependent upon several factors, including stability, cost, ease of product development, and experience with its use in formulation. Moreover, physicochemical factors such as toxicity potential, miscibility, solvent capacity, and dispersibility are also taken into consideration.15 Surfactants are composed of a hydrophilic and hydrophobic portion that is capable of improving drug solubility through a cosolvent effect or formation of micelles.21 Non-ionic surfactants are commonly used in lipid-based drug delivery systems. These can be categorized as either water-insoluble or water-soluble, in which the capacity to form micelles is low or high, respectively. Although the capacity for micelle formation is low, water-insoluble surfactants have enough hydrophilic character to undergo self-emulsification. Lipid excipients in combination with surfactants drive emulsification.22 The use of polyoxyl 40 hydrogenated castor oil or Cremophor® RH 40 has been used in the reformulation of cyclosporin A to increase oral bioavailability from 10% to approximately 20% to 50% higher with the inclusion of a surfactant.21 It is evident that surfactants can be used to improve the formulation of SLN successfully. Cosolvents are mixtures of miscible solvents that are used to solubilize poorly water soluble drugs.21 They are used in SLN preparation to increase drug dissolution and solvent capacity. In systems containing a high concentration of water-soluble surfactants, cosolvents are utilized to assist in dispersion.15 Commonly used cosolvents include PEG, glycerol, and propylene glycol. Additives such as antioxidants may be incorporated into SLN. Certain lipid and surfactant excipients are vulnerable to oxidation, which leads to gelatin cross-linking. This negatively affects SLN stability and impairs drug release.22 Thus, these antioxidants are useful in the prevention of oxidation of both the drug and the unsaturated fatty acid components of the SLN.15 Examples of antioxidants utilized in the preparation of SLN are propyl gallate, α-tocopherol, and butylated hydroxytoluene.
References
- Müller RH, Mäder K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery—a review of the state of the art. Eur J Pharm Biopharm. 2000;50(1):161-177.
- Martins S, Sarmento B, Ferreira DC, Souto EB. Lipid-based colloidal carriers for peptide and protein delivery— liposomes versus lipid nanoparticles. Int J Nanomed. 2007;2(4):595-607.
- Bunjes H. Lipid nanoparticles for the delivery of poorly water-soluble drugs. J Pharm Pharmacol. 2010;62(11):1637-1645.
- Fricker G, Kromp T, Wendel A, et al. Phospholipids and lipid-based formulations in oral drug delivery. Pharm Res. 2010;27(8):1469-1486.
- Grana A, Limpach A, Chauhan H. Formulation considerations and applications of solid lipid nanoparticles. Am Pharm Rev. 2013;16(1):19-25.
- Wissing SA, Kayser O, Müller RH. Solid lipid nanoparticles for parenteral drug delivery. Adv Drug Deliv Rev. 2004;56(9):1257-1272.
- Mehnert W, Mäder K. Solid lipid nanoparticles: Production, characterization and applications. Adv Drug Deliv Rev. 2001;47(2–3):165-196.
- Blasi P, Giovagnoli S, Schoubben A, Ricci M, Rossi C. Solid lipid nanoparticles for targeted brain drug delivery. Adv Drug Deliv Rev. 2007;59(6):454-477. doi:http://dx.doi.org.cuhsl.creighton.edu/10.1016/j.addr.2007.04.011
- Kathe N, Henriksen B, Chauhan H. Physicochemical characterization techniques for solid lipid nanoparticles: Principles and limitations. Drug Dev Ind Pharm. 2014;40(12):1565-1575.
- Prasad D, Chauhan H, Atef E. Studying the effect of lipid chain length on the precipitation of a poorly water soluble drug from self-emulsifying drug delivery system on dispersion into aqueous medium. J Pharm Pharmacol. 2013;65(8):1134-1144.
- Joshi MD, Müller RH. Lipid nanoparticles for parenteral delivery of actives. Eur J Pharm Biopharm. 2009;71(2):161-172.
- Uner M, Yener G. Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives. Int J Nanomed. 2007;2(3):289-300.
- O’Driscoll CM, Griffin BT. Biopharmaceutical challenges associated with drugs with low aqueous solubility—the potential impact of lipid-based formulations. Adv Drug Deliv Rev. 2008;60(6):617-624.
- Shah M, Agrawal Y. High throughput screening: an in silico solubility parameter approach for lipids and solvents in SLN preparations. Pharm Dev Technol. 2013;18(3):582-590.
- Pouton CW, Porter CJH. Formulation of lipid-based delivery systems for oral administration: materials, methods and strategies. Adv Drug Deliv Rev. 2008a;60(6):625-637.
- Heurtault B, Saulnier P, Pech B, Proust J, Benoit J. Physico-chemical stability of colloidal lipid particles.Biomaterials. 2003;24(23):4283-4300.
- Marsac P, Shamblin S, Taylor L. Theoretical and practical approaches for prediction of drug polymer miscibility and solubility. Pharm Res. 2006;23(10):2417-2426.
- Yuan X, Sperger D, Munson EJ. Investigating miscibility and molecular mobility of nifedipine-PVP amorphous solid dispersions using solid-state NMR spectroscopy. Mol Pharm. 2014;11(1):329-337.
- Chauhan H, Hui-Gu C, Atef E. Correlating the behavior of polymers in solution as precipitation inhibitor to its amorphous stabilization ability in solid dispersions. J Pharm Sci. 2013;102(6):1924-1935.
- Chauhan H, Kuldipkumar A, Barder T, Medek A, Gu CH, Atef E. Correlation of inhibitory effects of polymers on indomethacin precipitation in solution and amorphous solid crystallization based on molecular interaction.Pharm Res. 2014;31(2):500-515.
- Strickley R. Solubilizing excipients in oral and injectable formulations. Pharm Res. 2004;21(2):201-230.
- Hauss DJ. Oral lipid-based formulations. Adv Drug Deliv Rev. 2007;59(7):667-676.
Author Biographies
Anne Trivino is a graduate student pursuing a Doctorate of Pharmacy and Master of Science in Pharmaceutical Sciences at Creighton University, Omaha, NE. She received her Bachelor of Science in Molecular and Cellular Biology from the University of Illinois, Urbana- Champaign, IL.
Dr. Harsh Chauhan is an Assistant Professor at Creighton University, Omaha, NE. Dr. Chauhan received his PhD in Pharmaceutics from MCPHS, Boston, MA. His research focuses on amorphous systems and solid lipid nanoparticles. He worked as a visiting scientist at Vertex pharmaceuticals, and his professional affiliations include AAPS, ACS, and AACP. Contact: [email protected]